The Brain Disease Model of Addiction
Butler Center for Research - May 2021

Download the Brain Disease Model of Addiction Research Update.
Views and opinions on addiction have gone through many changes. Advances in neuroscience have helped us understand how drugs affect the brain, leading to the recognition that addiction is a chronic brain disorder that can be treated.1 The brain disease model of addiction is less stigmatizing than the view of addiction as a moral failing, and it brings hope that medications can be developed to address the disease.2 There is strong evidence supporting this paradigm, with neuroscientific research pointing to observable brain changes.2
The Brain Disease Model of Addiction Explained
The brain has many regions that are interconnected with one another, forming dynamic networks that are responsible for specific functions. Drugs can alter important brain areas that are necessary for healthy social interactions and life-sustaining functions, and can drive the compulsive drug use that marks addiction.1, 3, 4, 5
Addiction can be described as a repeating cycle with three stages. Each stage is associated with specific brain regions. The three-stages of addiction are:3, 4
- Binge/Intoxication: an individual uses an intoxicating substance and experiences its rewarding or pleasurable effects
- Withdrawal/Negative Affect: an individual experiences a negative emotional state in the absence of the substance
- Preoccupation/Anticipation: an individual seeks substance use again after a period of abstinence
The three stages are linked to each other, but they also involve different brain regions, circuits (or networks), and neurotransmitters; and result in specific kinds of changes in the brain. Brain areas affected by drug use include the basal ganglia, the extended amygdala, and the prefrontal cortex.1, 3, 4, 5
- The basal ganglia control the rewarding effects of substance use and are also responsible for the formation of habitual substance taking. These areas form a key node of what is sometimes called the brain’s "reward circuit." Drugs overstimulate this circuit, producing the euphoria of the drug high. But with repeated exposure, the circuit adapts to the presence of the drug, diminishing its sensitivity and making it hard to feel pleasure from anything besides the drug.
- The extended amygdala is involved in stress and the feelings of unease, anxiety and irritability that typically accompany substance withdrawal. This circuit becomes increasingly sensitive with increased drug use. Over time, a person with substance use disorder uses drugs to get temporary relief from this discomfort rather than to get high.
- The prefrontal cortex is involved in executive function (i.e., the ability to organize thoughts and activities, prioritize tasks, manage time, and make wise decisions), including exerting control over substance taking. This is also the last part of the brain to mature, making teens most vulnerable. Shifting balance between this circuit and the circuits of the basal ganglia and extended amygdala makes a person with a substance use disorder seek the drug compulsively with reduced impulse control.
Figure 1. The Three Stages of the Addiction Cycle and the Brain Regions Associated with Them
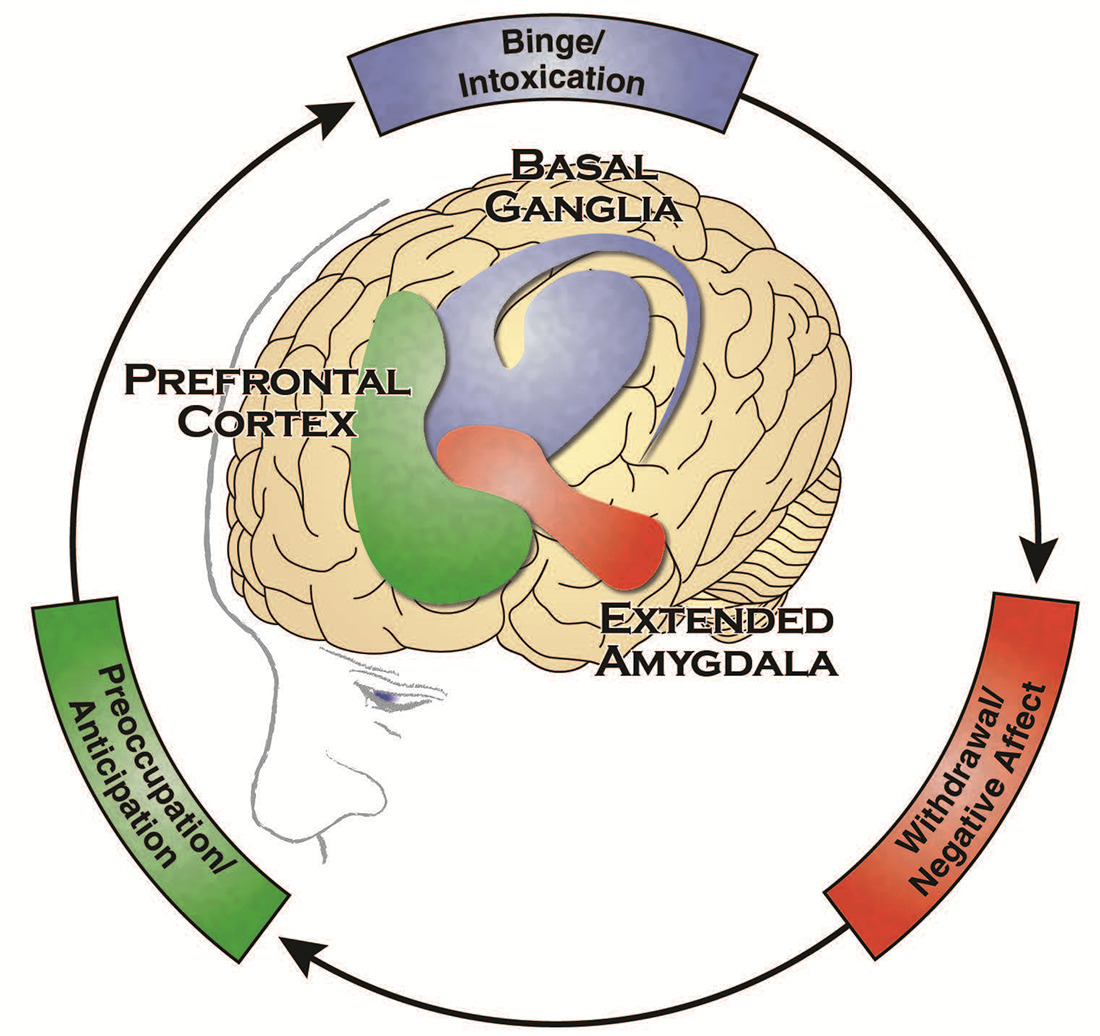
Source: Office of the Surgeon General, Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health
In addition to the neurobiological changes, the brain disease model of addiction also notes that many genetic, environmental and social factors contribute to an individual's vulnerability to begin using drugs, to continue using drugs and to undergo the progressive changes in the brain that characterize addiction. Factors that increase vulnerability to addiction include unaddressed trauma (sexual abuse, violence and adverse childhood experiences), family history of drug use, early exposure to drug use (adolescence is among the periods of greatest vulnerability to addiction), exposure to high-risk environments (typically, socially stressful situations with poor family and social supports, and environments in which there is easy access to drugs and permissive normative attitudes toward drug taking), and certain mental illnesses (e.g., mood disorders, attention deficit-hyperactivity disorder, psychoses and anxiety disorders).1, 3, 4, 18
Substance Use Disorder Treatment and Brain Research
The brain disease model of addiction has led to improvements in the understanding and treatment of substance use disorders. Identification of neural systems and structures that are changed by drug and alcohol use allow for development of different medication and non-medication-based treatments that target those vulnerable areas of the brain.3
Additional work on genetics (e.g., the study of genes) and epigenetics (e.g., the study of the impact of the environment on whether or not genes are expressed) have helped develop evidence of biomarkers (e.g., measures that capture what is happening in a cell at a given moment) that directly or indirectly affect the neurobiological processes that are involved in developing addictions.1, 6 Identifying biomarkers associated with drug- and alcohol-seeking behaviors will help to refine possible treatments and prevention of substance abuse.8, 9, 10
For example, scientists recently performed a genome-wide association study to try to identify genes that might put people at risk for problematic cannabis use. They identified a genetic locus on chromosome 8 that controls the levels of the gene CHRNA2 expressed in the brain. Low levels of expression of the gene CHRNA2 in the cerebellum are found to be associated with cannabis use disorder, including diagnosis at an earlier age. The findings suggest that under-expression of CHRNA2 in the cerebellum (and probably other brain regions) is involved in cannabis use disorders, and provides a potential target for future prevention strategies, therapies and medication.7, 11
Critiques of the Brain Disease Model of Addiction
One criticism of the brain disease model of addiction is that it does not reduce the moral stigma attached to addiction and may instead attach a new stigma by using the word disease.12 Critiques of this model also include that it may cause feelings of helplessness for those struggling with addiction, and it ignores other factors involved in developing and sustaining the negative behaviors of substance use disorders.12, 13, 14, 15, 16
However, research does not support these criticisms, and rather than disregarding psycho-social factors, the brain disease model attempts to explain how the environment and individual differences are a part of the development of addiction as a brain disease.1, 3
Conclusion
The brain disease model of addiction has contributed greatly to the current view of substance use disorders. Understanding the neurobiological changes that the brain undergoes has allowed for developments of novel intervention and prevention methods, while also providing overall stigma reduction. Continued advances in neuroscience research will serve to provide new and effective ways to combat the disease of substance use disorders.
Questions
Question: Why is it beneficial to understand the brain disease model of addiction?
Response: Advances in neuroscience and imaging technology have quickly evolved our understanding of addiction and demonstrated support for the brain disease model of addiction. A disease view of addiction with neuroscientific research pointing to observable changes in the brain can be seen as much less stigmatizing and has allowed for the development of different interventions, both medication and non-medication-based, that target vulnerable neuronal circuits. This model considers genetic and environmental factors that cause physical changes to the brain and significantly increases the core understanding of addiction that may lead to more precise and effective treatment options.
How to Use This Information
For patients: Addiction can be treated, and no matter what genetic characteristics you may have, physical changes in the brain can be reversed through sustained abstinence. The brain has an amazing ability to change and heal itself in response to mental experience, known as neuroplasticity. The brain is not fixed and unchangeable, but can create new neural pathways to adapt to its needs.17 If you have been unsuccessful with behavioral interventions alone, medication-assisted treatment can help address physical parts of the addiction while you learn critical new behaviors, examine unhealthy attitudes, and address important environmental factors through a treatment program.
For friends and family: When supporting loved ones with addiction, it is important to remember that their dependence is not a result of character, nor is it something they can "just quit." Addiction is a complicated and multifaceted disease with physical, social and psychological components, much like diabetes or heart disease. Sustained abstinence from alcohol and other drugs can reverse the physical damage caused by addiction, and this requires intensive participation in a holistic treatment program, especially for those whose genetic brain structure makes them more prone to substance dependence.
References
- Volkow, N. D., Michaelides, M., & Baler, R. (2019). The neuroscience of drug reward and addiction. Physiological Reviews, 99(4), 2115–2140. doi:10.1152/physrev.00014.2018
- Heilig, M., MacKillop, J., Martinez, D., Rehm, J., Leggio, L., & Vanderschuren, L. J. M. J. (2021). Addiction as a brain disease revised: Why it still matters, and the need for consilience. Neuropsychopharmacology, 1–9. doi.org/10.1038/s41386-020-00950-y
- Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. The New England Journal of Medicine, 374(4), 363–371. doi:10.1056/NEJMra1511480
- Office of the Surgeon General. (2016). Facing addiction in America: The Surgeon General's report on alcohol, drugs, and health. addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf
- National Institute on Drug Abuse. (2020). Drugs, brains, and behavior: The science of addiction.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain
- Edwards, D., Roy, A. K., 3rd, Boyett, B., Badgaiyan, R. D., ... Blum, K. (2020). Addiction by any other name is still addiction: Embracing molecular neurogenetic/epigenetic basis of reward deficiency. Journal of Addiction Science, 6(1), 1–4.
- National Institute on Drug Abuse. (2019). Drug Facts: Genetics and epigenetics of addiction. drugabuse.gov/sites/default/files/genetics _and_epigenetics_drugfacts_2.pdf
- Kwako, L. E., Bickel, W. K., & Goldman, D. (2018). Addiction biomarkers: Dimensional approaches to understanding addiction. Trends in Molecular Medicine, 24(2), 121–128. doi.org/10.1016/j.molmed.2017.12.007
- Volkow, N. D., & Boyle, M. (2018). Neuroscience of addiction: Relevance to prevention and treatment. The American Journal of Psychiatry, 175(8), 729–740. doi:10.1176/appi.ajp.2018.17101174
- Volkow, N. D., Koob, G., & Baler, R. (2015). Biomarkers in substance use disorders. ACS Chemical Neuroscience, 6(4), 522–525. doi.org/10.1021/acschemneuro.5b00067
- Demontis, D., Rajagopal, V. M., Thorgeirsson, T. E., Als, T. D., ,... Børglum, A. D. (2019). Genome-wide association study implicates CHRNA2 in cannabis use disorder. Nature Neuroscience, 22(7), 1066–1074. doi:10.1038/s41593-019-0416-1
- Frank, L. E. & Nagel, S. K. (2017). Addiction and moralization: The role of the underlying model of addiction. Neuroethics, 10(1), 129–139. doi:10.1007/s12152-017-9307-x
- Carreno, D. F. & Pérez-Escobar, J. A. (2019). Addiction in existential positive psychology (epp, pp2.0): From a critique of the brain disease model towards a meaning-centered approach. Counseling Psychology Quarterly, 32(4):1-21. Advance online publication. doi:10.1080/09515070.2019.1604494
- Hall, W., Carter, A., & Forlini, C. (2015). The brain disease model of addiction: Is it supported by the evidence and has it delivered on its promises? The Lancet Psychiatry, 2(1), 105–110. doi:10.1016/S2215-0366(14)00126-6
- Lewis, M. (2018). Brain change in addiction as learning, not disease. The New England Journal of Medicine, 379(16), 1551–1560. doi:10.1056/NEJMra1602872
- Lewis, M. (2017). Addiction and the brain: Development, not disease. Neuroethics, 10, 7–18. doi:10.1007/s12152-016-9293-4
- Shaffer, J. (2016). Neuroplasticity and clinical practice: Building brain power for health. Frontiers in Psychology, 7, 1118. doi:10.3389/fpsyg.2016.01118
- Dube, S. R., Felitti, V.J., Dong, M., Chapman, D. P., Giles, W. H., & Anda, R. F. (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The Adverse Childhood Experiences Study. Pediatrics, 111(3), 564–572. doi:10.1542/peds.111.3.564
